How Is a Food Allergy Different from an Intolerance?
Food allergies and intolerances, and food allergy testing are some of the most misunderstood issues in medicine, both by doctors and the general public. In order to understand the differences between various food allergy and intolerance tests, unfortunately you have to understand how the words “intolerance” and “allergy” are being defined differently by different groups of people. Then you have to understand what is actually being measured in these tests, and finally the science (or lack thereof) being applied in various tests. It’s a very complex topic.
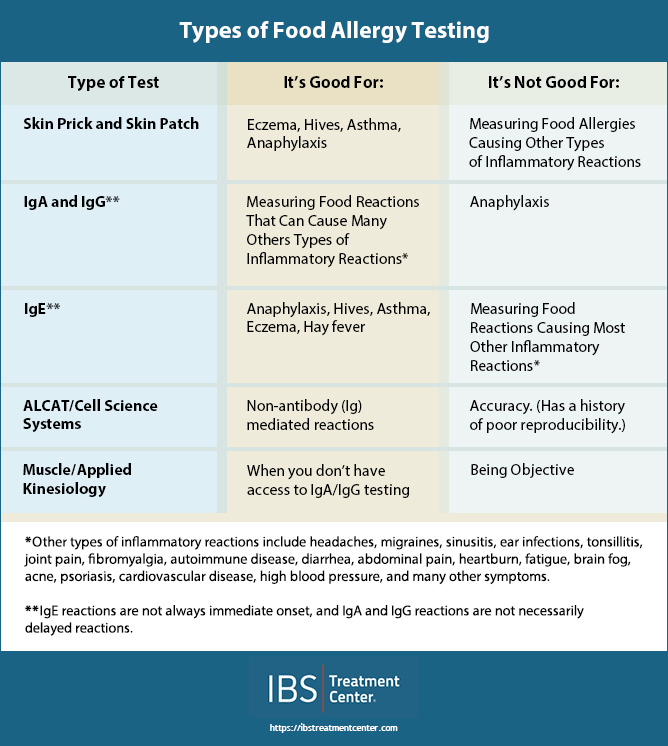
I’ve summarized it in the graphic above, but if you really want to know the details, keep reading.
To begin, there is debate about what even constitutes a food allergy. The full scientific definition of food allergy includes any immune reaction to a food. However, traditional allergy specialists have in more recent years redefined allergy for their convenience as being only one type of immune reaction with a very limited number of possible symptoms.
This definition of food allergy only includes immunoglobulin Type E (IgE) reactions, which are produced by the immune system, and excludes symptoms other than asthma, eczema, hay fever, hives, rashes, and anaphylaxis. These reactions must occur within a short time (minutes) after exposure to the food. Any other IgE reaction is conveniently ignored, including any blood work positive for IgE antibodies that cannot be associated with one of these symptoms. This redefinition of food allergy was done for convenience and is used by most allergists today, but it is highly subjective and ignores the majority of allergic reactions to food.
Research does not demonstrates that food allergies (immune system reactions to foods) are limited to these symptoms, and there are many studies that demonstrate that immune reactions, IgE and others, can be delayed by hours, days, and even longer, and can produce a wide variety of symptoms. Thus, many statements made by physicians and physicians groups concerning food allergies must be understood to only be relevant within a very narrow definition of food allergy, as described above.
Studies have demonstrated that other immune reactions, such as immunoglobulin type G (IgG) antibodies to foods indicate allergies and can produce all types of inflammatory symptoms, including migraine headaches and joint pain. Other studies have demonstrated that such allergies can produce IBS-type digestive symptoms as well as many other symptoms.
Many people claim that celiac disease is not an allergy because we refer to it as a gluten intolerance. This leads to even more confusion. One would then assume that if gluten is an intolerance, the immune system isn’t involved in the reaction. But studies on celiac disease have shown that celiac disease is clearly an immune reaction, and symptoms are generally eliminated by ending the exposure to gluten.
The word “intolerance” is also used with lactose intolerance, which is well understood to be a deficiency in the enzyme required to digest lactose. There is no immune reaction in a lactose intolerance. Contrast that with a gluten intolerance, which is not an enzyme deficiency and definitely involves the immune system. Yet both are referred to as intolerances. All of this confusion is due to an unfortunate lack of clarity and even the lack of any standards at all when it comes to the use of the words “allergy,” “intolerance,” and even “sensitivity.”
Most people who do have a reaction to dairy assume that it’s a lactose intolerance. This may be true, or it may be a dairy allergy. A lactose intolerance, as previously stated, is an enzyme deficiency and does not involve the immune system. Therefore, it does not cause inflammation. It only causes very temporary digestive symptoms and those symptoms are limited to the digestive tract.
A dairy allergy, however, is an inflammatory reaction that involves the immune system. It can cause the same digestive symptoms as a lactose intolerance, and it can also cause wide ranging symptoms throughout the body, such as congestion, sinusitis, headaches, fatigue, and many other symptoms.
Other confusion around what constitutes an allergy involve false claims about how some immune reactions are special, and that some immune reactions are even necessary to protect us from food. Statements have been made that IgG or IgA antibodies (two other types of immunoglobulins produced by the immune system) are produced by everyone on exposure to any food, thus indicating tolerance to that food. However, it is clear that most people do not produce antibody reactions to most foods. And the idea that these antibodies are necessary, protect us from food, or that they indicate tolerance, are not supported by clinical experience or by published research.
Unfortunately, the medical community lags far behind the public on this topic. We should have clear and logical definitions for all types of food allergy, intolerance, and sensitivity. There should also be a major emphasis to follow-up on the studies that have demonstrated the value of identifying atypical food allergies through reliable, repeatable lab testing, so that we can continue to learn more about the incredibly important impact that they have on creating inflammation and their role in the development of chronic disease.
Why You Should Do Food Allergy Testing
For approximately twenty years we have had the unique distinction of testing thousands and thousands of patients for food allergies and have received their feedback on how much impact those food allergies have been having on their health. The results reported by patients have been overwhelming and profound. Most patients discover that they have been unknowingly suffering for years from a food allergy, and they report that the removal of that food from their diet has dramatically improved their health.
We are now certain that this type of testing is vitally important to understanding an underlying cause of inflammation that leads to many digestive problems and other chronic diseases suffered by millions of people. The limiting factors for this kind of testing is the quality control at the lab, the skill level of the healthcare provider interpreting the results, and the subsequent education of the patient on how to implement those results.
The ingestion of foods does lead to an immune response in the body of a healthy person. If a substance in your body is not causing a problem, your body will not form an immune response (make antibodies) against it. However, once the immune system starts to create antibodies against something, it doesn’t usually stop until that substance is gone. This is the same for food as it is for a virus or a bacteria. And this immune response leads to a cascade of events that cause inflammation, and will continue to cause inflammation until the trigger is removed.
Which Foods Should You Test?
there are many different foods that can be tested, but they should include the majority of the foods in your diet. In general, a person should be tested for reactions to at least a hundred different kinds of foods
Comprehensive food allergy testing may include testing for reactions to the following:
- Dairy: cow’s milk, whey, casein, mozzarella cheese, cheddar cheese, cottage cheese, yogurt, goat’s milk
- Meat and Poultry: beef, chicken, lamb, pork, chicken, turkey, chicken egg white, chicken egg yolk, duck egg
- Grains: amaranth, barley, buckwheat, corn, gliadin (wheat), gluten (wheat), oat, rice, rye, spelt, whole wheat
- Seafoods: lobster, clam, cod, crab, halibut, scallop, salmon, shrimp, red snapper, sole, tuna
- Vegetables: avocado, broccoli, beet, green bell pepper, cabbage, carrot, cauliflower, celery, cucumber, garlic, lettuce, mushroom, olive (black), onion (white), potato (white), pumpkin, radish, spinach, sweet potato, tomato, zucchini squash
- Nuts: almond, coconut, hazelnut, peanut, pecan, sesame seed, sunflower seed, walnut
- Legumes: green pea, kidney bean, lentil, lima bean, peanut, pinto bean, string bean, soy bean
- Fruits: apple, apricot, banana, blueberry, cherry, grape (red), grapefruit, lemon, orange, papaya, peach, pear, pineapple, plum, raspberry, strawberry
- Miscellaneous: coffee bean, cocoa (chocolate) bean, honey, baker’s yeast, brewer’s yeast, sugar cane
What Different Types of Tests Can (and Can’t) Tell You
There are several different types of allergy tests. These tests are not the same, do not tell you the same things, and do not measure the same types of reactions. Before forming an opinion about a test, we must understand its strengths and its limitations. In order to define the different types of food allergy testing we have to look deeper than just the name of the test. That is simply marketing. The capabilities of the test are determined by the underlying methods used by the test to detect the reaction, and the quality control done at the lab to make sure that this complex testing is accurate.

Skin Testing
For several decades, skin prick and skin patch testing have been the standard ways to test for allergies. If you visit a traditional allergist, you will likely undergo this type of testing. The potential allergen is injected under or scratched into the skin, and any resulting inflammation, also known as a wheal, is measured. The size of the wheal determines whether or not an allergy is diagnosed.
In theory, skin tests measure IgE antibody reactions. Skin testing seems to be relatively good for evaluating some skin reactions, such as some eczema, hives, and rashes, asthma, and anaphylaxis. In reality, skin tests do not correlate very well with IgE blood tests and are often negative, missing elevated IgE blood tests. This type of testing is ineffective at deducing most other types of food allergies. It also leaves a lot to be desired because we don’t inject food into our skin when we eat, nor do we necessarily get a red bump when we have a food allergy. It is useful for some types of food allergies, but not most.
For example, a gluten intolerance won’t show up on skin testing. In fact, allergy doctors don’t even get involved in diagnosing a gluten intolerance, because it is considered a digestive issue. This is in spite of the fact that a gluten reaction can cause skin problems and many other symptoms, not just digestive symptoms.
Another challenge with skin testing is that many people are incorrectly told after skin testing that they do not have a food allergy because it was negative on the skin test. Other people seem to react to everything that is tested because their skin is extremely sensitive to being pricked. Either way, skin testing is far from perfect. Skin testing is probably most relevant for life threatening or anaphylactic types of food allergies.
IgE Blood Test
IgE blood testing is also valuable, and for more than just these symptoms. Some people have symptoms caused by IgE reactions that are not asthma, eczema, hives, rash or anaphylaxis. Therefore, it can be beneficial to test for IgE antibodies even when these symptoms are not present.
IgA and IgG Blood Test
At least as important as skin testing is measuring IgA and IgG antibodies. These tests tend to call themselves food intolerance tests rather than food allergy tests, just to avoid having to explain that they are really just a different type of allergy test.
This type of testing is much better at finding food allergens that cause symptoms other than those more often seen with skin testing. However, IgA and IgG reactions can also lead to eczema, rashes, hives, asthma and occasionally even anaphylaxis. This testing is done via the blood. (There is another type of antibody, secretory IgA, that can be found in saliva and stool samples. Secretory IgA antibodies also have value in diagnosing food allergens.)
IgA and IgG antibodies are two different types of immune responses, and they will not necessarily both be elevated when one or the other is elevated. If either one is elevated, it indicates an inflammatory reaction and should be taken seriously.
Sometimes the word “ELISA” is associated with these types of tests. ELISA is a detection method often used for measuring these antibodies. It is a very well-established testing method and is the same detection method used in many types of tests, such as tests for viruses, hepatitis, and even the pregnancy test. It is a test method and should not be confused with the name of the test itself.
ELISA testing is used throughout the medical field in a variety of applications and is highly reproducible when run by a quality lab with high quality control standards. It is not a simple testing method, but it is very scientific and very accurate when done properly.
There are many double-blind placebo-controlled studies that have demonstrated the accuracy of this type of testing. ELISA testing can measure any antibody including IgE, IgG, and IgA. All three have the potential to cause inflammation and therefore the potential to cause symptoms in patients.
Antibody testing does have many challenges. The biggest challenge is that there are many steps that must be carefully performed in order to accurately measure antibodies. When ELISA technology is not done carefully and with excellent quality control, it can produce inaccurate results. Therefore, it must be run by a lab that has a keen focus on quality control and reproducibility. Many labs that do antibody testing do not put enough emphasis on quality control and their lab work may not be reliable.
Another problem many patients encounter is when they ask a doctor who is not familiar with this type of testing for an opinion on how to interpret the results. It is not uncommon for a physician to offer their opinion or advice on what the test means, when in fact they have no experience with these tests or training on how to interpret these tests.
These challenges often give people cause to suspect that their IgA or IgG antibody testing is not accurate does not have value. However, when done well, it’s just as accurate as any other blood test, many of which also use ELISA technology, and provides an immense amount of information about your health.
Cell Mediated Tests
Another type of food sensitivity testing on the market is defined by a completely different type of technology. This testing is best known by its brand name, often going under the name ALCAT or Cell Science Systems. These tests tend to call themselves food sensitivity tests rather than food allergy tests, but in reality they are another type of food allergy testing. These tests are also blood tests, but they do not measure antibodies.
These tests are based on the theory that the size of your white blood cells can be affected by the introduction of food into your blood. When this is done in the lab, changes in the size of your white blood cells can be measured and are hypothesized to represent an immune reaction to the food. There is no precedent for this type of testing in the conventional medical world, but it is an interesting hypothesis and some people have found this testing helpful.
The most concerning issue with this type of testing is that in both published and clinical reproducibility studies, this type of testing had very poor reproducibility when split samples of the same blood were sent to the lab. This means that identical samples from the same patient on the same day returned different results.
This is troubling, to say the least. If you can’t trust the results, then maybe the test method is too challenging to perform routinely. This type of testing is interesting, and the technology may have potential, but it’s current value is questionable.
Muscle Testing/Applied Kinesiology
Finally, there is muscle testing. Muscle testing, also known as muscle energy testing or applied kinesiology, is the act of holding a substance like a food and then having a practitioner pull down on your outstretched arm to determine your ability to resist their pressure. The theory is that your strength will weaken if the substance does not mesh with your energy field.
This technique was developed by practitioners who could not draw blood nor run other types of testing, but who apparently saw a connection between food and health. It may sound strange, however many people claim to have been helped through muscle energy testing, and the number of people who practice this type of testing is significant.
There may very well be something to the idea that our energy is affected by various substances, and you may find this testing helpful. Unfortunately there are no studies comparing this type of testing to other types of testing. But it would not be wise to underestimate the effect that food can have on your body.
Who Should be Tested?
There is scientific evidence to demonstrate food allergies can cause migraines, digestive problems, joint pain, mood disorders, skin problems, and many other conditions, even heart disease. Clinically we’ve seen all of this and many other problems caused or exacerbated by food allergies. These include chronic sinusitis, ear infections, acne, headaches, fatigue, weight gain, depression, environmental allergies, eczema, fibromyalgia, insomnia, brain fog, and many others.
In our opinion everyone should be tested for food allergies. This would solve endless numbers of people suffering from chronic disease and save millions of dollars a year in healthcare costs. As a culture we should focus on increasing our understanding of food allergies so that we can help more people benefit from this amazingly simple yet profound treatment. We highly recommend that you get tested for food allergies and get the right kind of testing.
Since 2005 the IBS Treatment Center has successfully tested and treated thousands of patients of all ages, from infants to seniors. Solving IBS is our expertise, and along the way we’ve discovered that we’ve incidentally helped solve thousands of other health problems from which patients were suffering. One of the key steps is the proper testing for food allergies. Contact us today to get started solving your problem.

Dr. Wangen is the founder and medical director of the IBS Treatment Center, the award winning author of two books, and a nationally recognized speaker on digestive disorders. He has been on ABC, NBC, and Fox as well as public radio, and was named one of Seattle’s Top Doctors by Seattle Magazine.